
Living with a Spinal Cord Injury 
When I woke up in recovery after my surgery to remove a tumor on my spine, it took me a while to adjust to the feelings that I no longer had in my body and the realization that there were going to be many things that I could no longer do with my body. Not being able to go to the toilet on my own and being dependent on a catheter and then a bed pan was the hardest thing to accept.
The first time that I was able to get in and out of a wheelchair was the realization that this injury was going to be permanent or at least a very long term disability. It was about a week after my surgery that I was visited by representatives from the Ontario Spinal Cord Injury Association. They gave me a book to read (Life after a Spinal Cord Injury) which I put aside at first–my denial–but I later read from cover to cover twice over. With support from my family, friends and people I have met on my journey, I am learning to accept my spinal cord injury.
Not everyone with a spinal cord injury ends up in a wheelchair or having to use ambulatory assists. However, that does not mean that you are not suffering from a SCI. You may still have limited mobility such as not being able to rotate your head from side to side as the result of a fractured C1-C2. Many people are able to continue with their lives, walking, running, jogging, holding down existing jobs, driving, and living life as they did before their SCI with just a few adjustments. On the other hand, many are not so lucky and this chapter on my website is mainly for those that are seriously affected by a spinal cord injury.
For me, researching and understanding the full extent of what a spinal cord injury is and how to live with all those aspects that I was facing is what I am extending to you here.
TABLE OF CONTENTS
- Understanding the spine
- What is a spinal cord injury?
- What are the symptoms of a spinal cord injury?
- What types of spinal cord injury are there?
- What types of paralysis are the results of an SCI?
- What symptoms will your health care team monitor?
- What does the road to recovery look like?
- Obstacles to overcome after a SCI.
- Keys to independence and rehabilitation.
“Recovery is not a race. You don’t have to feel guilty if it takes longer than you thought it would.”
— Anonymous
![]()
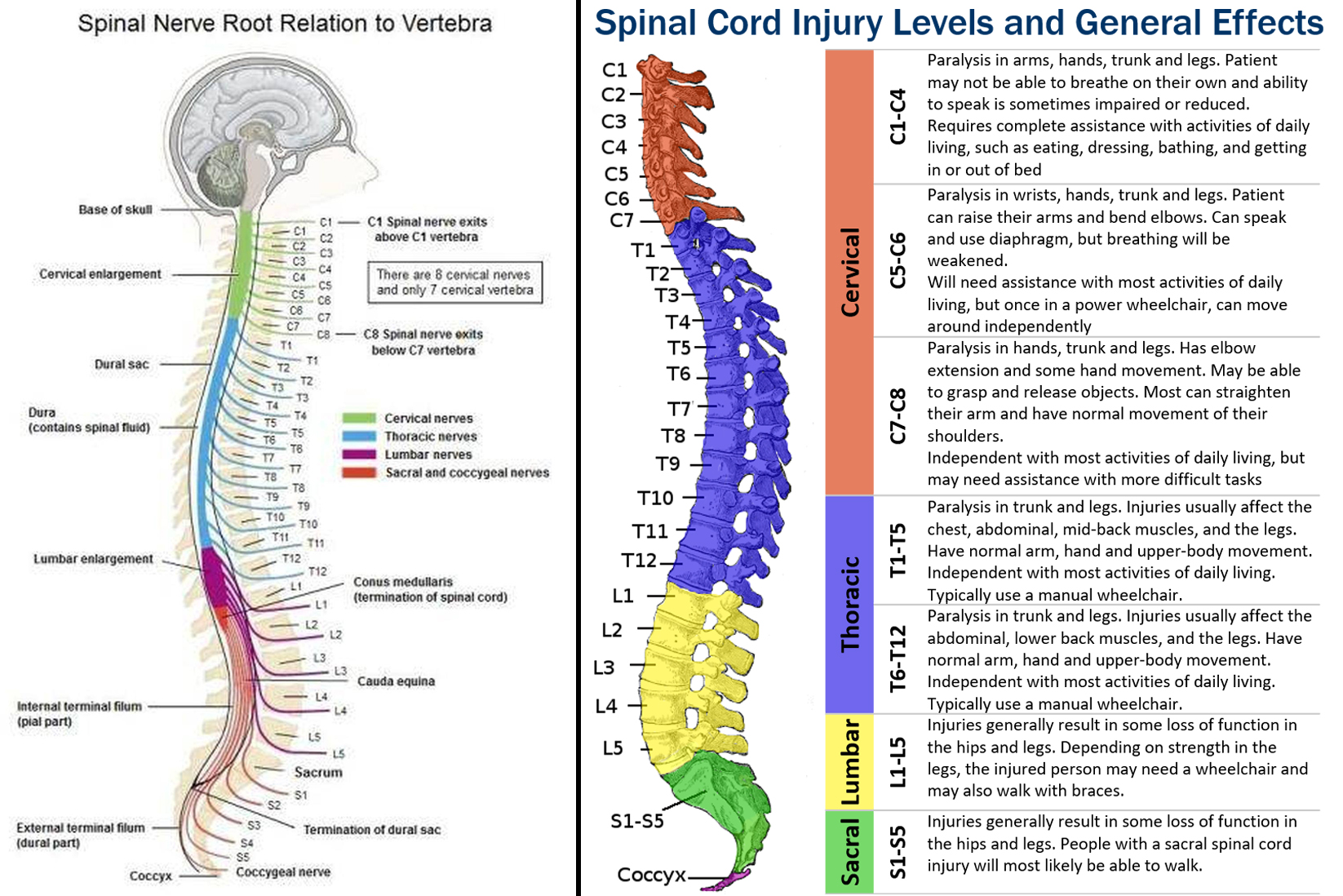
The spine is divided into six regions.
Cervical spine (the neck): The top part of the spine has seven vertebrae (C1 to C7). The neck vertebrae allow you to turn, tilt and nod your head. The cervical region of the spinal cord controls the movements and sensations of the neck, shoulders, arms, and hands. Injuries to this region can cause paralysis or weakness in these areas, as well as difficulty breathing and speaking.
Thoracic spine (the back): The thoracic part of the spine has twelve vertebrae (T1 to T12). The ribs are attached to the thoracic spine. The thoracic region of the spinal cord controls the movement and sensation of the chest, mid-back, and abdominal muscles. Injuries to this region can cause difficulty with breathing and coughing, and may also affect trunk stability and bowel and bladder control.
Lumbar spine (the lower back): The five vertebrae (L1 to L5) make up the lower part of the spine. The lumbar spine supports the upper parts of your spine. The lumbar region of the spinal cord controls the movement and sensation of the hips, legs, and feet. Injuries to this region can cause paralysis or weakness in the legs, as well as difficulty with bowel and bladder control.
Sacrum (the base of the spine): The five sacral vertebrae (S1 to S5) fuse (weld together) during fetal development, which means they don’t move. These bones carry the weight of the body and it is the site for many muscles and ligaments that attach to in the hip and pelvic.
Coccyx (the tailbone): There are Four fused vertebrae that make up this small piece of bone found at the bottom of your spine.
A spinal cord injury (SCI) or lesion, is damage to the bundle of nerves and nerve fibres that sends and receives signals from the brain. A SCI can be caused by direct injury to the spinal cord itself or from damage to the tissue and bones (vertebrae) that surround the spinal cord. This damage can cause temporary or permanent changes in feeling, movement, strength, and body functions below the site of injury.
A spinal cord injury involves damage to any part of the spinal cord which extends from the lower part of the brain down through the lower back. It can also include damage to nerves at the end of the spinal cord, known as the cauda equina. Since the spinal cord sends and receives signals between the brain and the rest of the body, an injury often causes permanent changes in strength, feeling and other body functions below the site of the injury.
“My mission in life is not merely to survive, but to thrive; and to do so with some passion,
some compassion, some humour, and some style.”
— Maya Angelou
![]()
What are the symptoms of a spinal cord injury?
The symptoms of a spinal cord injury depend on the extent and location of the injury. Paralysis can happen immediately upon injury (primary damage) or can develop over time from bleeding and swelling in the spinal cord and cell death (secondary damage). Damage to the spine can also be caused by infections or disease such as cancerous tumors.
A spinal cord injury can damage a few, many, or all of the nerve fibres that cross the site of injury. If the injury causes little or no nerve cell death, a person can make an almost complete recovery.
SCI can cause one or more symptoms, including:
- Numbness, tingling, or a loss of (or changes in) sensation in hands and feet
- Paralysis (loss of movement)
- Pain or pressure in the head, neck, or back
- Weakness in any part of the body
- Unnatural positions of the spine or head
- Loss of bladder and bowel control
- Problems with walking
- Difficulty breathing
- Changes in sexual function
What types of spinal cord injury are there?
An incomplete injury means the spinal cord is still able to send some messages to or from the brain. People with an incomplete injury may still have some feeling, function below the site of their injury.
- Retaining some sensation below the site of the injury. The sense of feeling may come and go, and may be much weaker than the sensations you used to experience.
- Being able to move some muscles below the site of the injury. The extent of movement may vary, and they may have good control over some muscles, but no control over others.
- Pain below the injury. Many incomplete spinal cord injury survivors report issues with chronic pain.
A complete injury means that there is no nerve communication below the injury site.
- Loss of sensation below the site of the injury.
- Complete loss of muscle control and motion below the site of the injury.
- Difficulty controlling your bladder and bowels.
- If the injury is high enough in your spinal cord, difficulty breathing on your own.
What types of paralysis are the results of an SCI?
Paraplegia is the result of an injury or lesion to the thoracic region of the spine. This paralysis affects all or part of the trunk, legs and pelvic organs but not the arms.
Quadriplegia or Tetraplegia is the result of an injury or lesion at the level of the neck or cervical vertebrae. This means that the arms, hands, trunk, legs and pelvic organs are all affected by your spinal cord injury.
The following video explains the different areas of the spine and what injuries to those areas mean.
"Recovery is not for people who need it; it’s for people who want it."
— Anonymous
![]()
What symptoms will your health care team monitor?
- Loss of movement.
- Loss of control in any part of the body.
- Weakness, loss of coordination.
- Trouble with balance and walking.
- Loss of or a change in sensation. Ability to feel heat, cold or touch.
- Numbness, tingling or loss of feeling in the hands, fingers, feet or toes.
- Stiffness and changes to muscle tone.
- Loss of bowel or bladder control.
- Exaggerated reflex activities or spasms.
- Circulatory changes, blood pressure, heart rate, blood oxygen levels.
- Pain or an intense stinging sensation caused by damage to the nerve fibres in the spinal cord.
- Trouble breathing, coughing or clearing secretions from the lungs.
- Pressure sores, also known as bed sores.
- Extreme back pain or pressure in the neck, head or back.
- Changes in sexual function, sexual sensitivity and fertility.
- Ongoing bloodwork to determine function of vital organs (liver, kidneys, spleen, pancreas, thyroid, etc.).
- Ongoing ultrasound tests to determine function of bladder and bowels.
"It’s not the load that breaks an individual down.
It’s the load they are not prepared for."
— Tim Gabbett
![]()
What does the road to recovery look like?
In a nut shell, it is all about taking care of yourself. Let's start with the outer you, your skin. These are probably the most important things you can do for yourself, by yourself.
The Skin: is the largest organ of the human body. It protects us from infections. It is a barrier against bacteria, water and foreign objects. Skin warns us of temperature changes, undue pressure and other stimuli that assault the body. The skin has a unique ability to heal itself (ecchymosis) from cuts, scratches, bruises and bumps. The skin eliminates alts, oils, water and other organic matter through sweat glands.
-
Hydrate: drink ample amounts of water to keep skin healthy
-
Moisturize: keep the skin well lubricated to keep the skin subtle and pliable.
-
Regulate body temperature: spray the skin with a fine mist to help regulate body temperature, especially if you are feeling hot or flushed. Common occurrence with paraplegia and quadriplegia.
-
Clothing: avoid wearing tight clothing or any clothing that can be restrictive. The body, through the skin, needs to breath. Do not stay long in wet clothing. Wear protective gloves when pushing your wheelchair to help prevent blisters, cuts, bruises and pressure sores.
-
Pressure sores (bed sores or decubitus sores) will first appear in the form of redness or a blister. If the patient is immobile, checking for sores should be done on a daily basis, otherwise regular body checks when washing or bathing should be adequate.
- Movement and exercise on a daily basis. Do not let the body be inactive for long periods of time.
- Relieve the pressure on the sore by elevating the area. Putting pillows or cushions around the affected area will help too.
- Practice good hyena to keep the body and areas where soars frequent clean and healthy.
- There are special wheelchair cushions, foam mattresses, inflatable mattresses and other items that are available from your local disability equipment providers.
"We must learn to listen to the signals our bodies send us."
— David Servan-Schreiber
![]()
Looking after you bladder and bowels.
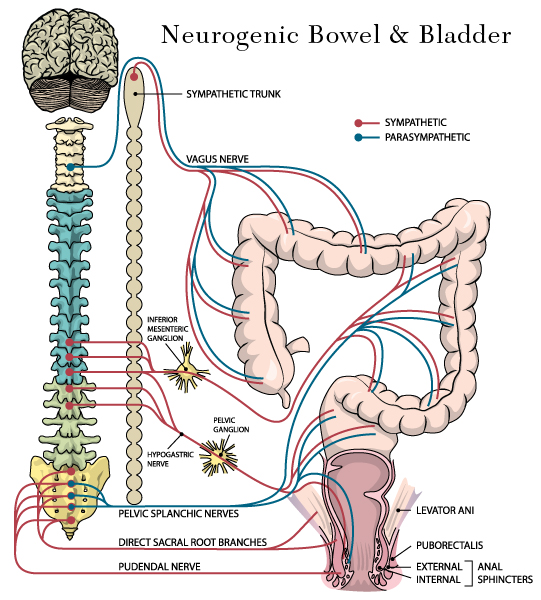 People that have been diagnosed as complete or incomplete, paraplegic or quadriplegic will all have issues with digestion and elimination especially if their injury is above the 12th thoracic and lumbar regions of the spine. These injuries change how peristalsis occurs. Sensation and voluntary control of muscles are affected.
People that have been diagnosed as complete or incomplete, paraplegic or quadriplegic will all have issues with digestion and elimination especially if their injury is above the 12th thoracic and lumbar regions of the spine. These injuries change how peristalsis occurs. Sensation and voluntary control of muscles are affected.
- Neurogenic bowel
- Neurogenic bladder
- Incontinence & frequent urination
- Bladder care and control after an SCI
- Bowel care and control after an SCI
- Rehabilitation & daily living
- Self-catheterisation – Women
- Self-catheterisation - Men
“What lies behind us and what lies before us are tiny matters compared to what lies within us.”
— Ralph Waldo Emerson
![]()
Breathing; the source of life!
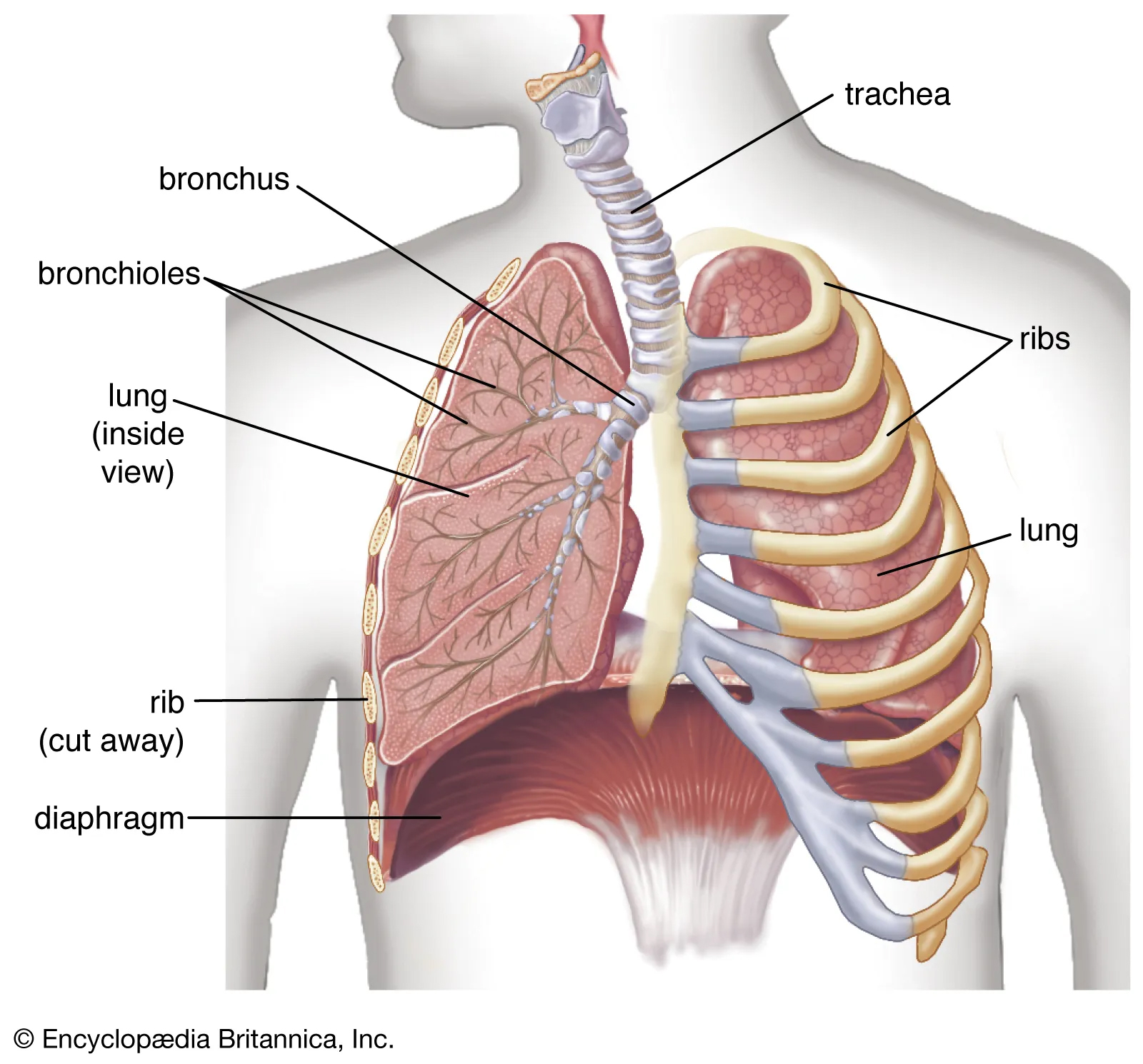 For people with a Spinal Cord Injury (SCI) respiratory dysfunction is common, especially with injuries occurring at the C1-C7 and T1-T7, which affect all functions below the site of injury.
For people with a Spinal Cord Injury (SCI) respiratory dysfunction is common, especially with injuries occurring at the C1-C7 and T1-T7, which affect all functions below the site of injury.
Lungs are organs suspended in the thoracic cage that fill with air as a result of the expansion of the thoracic cage, like bellows. Abdominal muscles force expirations, such as coughing. When the abdominal muscles relax, the thoracic cage collapses and the diaphragm returns to its normal position. In the case of a SPI these muscles may be compromised. Normal respiration for the average adult is 14 to 20 times per minute.
The most common complications of respiratory issues are: hypoxemia, hypercapnia, hypoventilation, mucous plugs, pulmonary edema, pulmonary embolism, pneumonia, apnea and decreased cardiac output due to diminished strength in the respiratory muscles.
Levels of the spine that affect breathing
- If the injury is located above the level of T12, the abdominal muscles are neurologically affected. This affects coughing and forced respiration and secretions can accumulate in the lungs.
- Above the level of T7 the intercostals muscles are affect. The cough function can be affected.
- Above C7, the accessory muscles are affected. The ability to cough is absent and lung capacity falls below 40%.
- Diaphragm is only affected with injuries at C5 or above.
- Neurological muscle damage occurs with injuries of C3 to C5.
- Complete injuries of the C1 and C2 will be dependent on a ventilator. Injuries of the C3 and above of the complete nature will more than likely require a ventilator.
Things you can do to help with breathing.
- Breath in through your nose; exhale through your mouth.
- Practice coughing.
- Practice deep breathing exercises.
- Practice meditation and mindfulness.
- Change positions often.
- Increase the humidity of your living space, especially where you sleep.
- Hydrate; increase fluid intake to prevent mucus build up.
- Remove environmental pollutants; cigarette smoke, allergens, and air pollution.
“When you arise in the morning, think of what a precious privilege it is to be alive,
to breathe, to think, to enjoy, to love.”
— Marcus Aurelius
![]()
Blood vessels in the paralyzed limbs lose their ability to expand and contract. This is a condition called vasodilatation, which is the widening of blood vessels. This happens when smooth muscles found in the walls of arteries or large veins relax, allowing the blood vessels to become more open. This leads to an increase in blood flow through your blood vessels as well as a decrease in blood pressure.
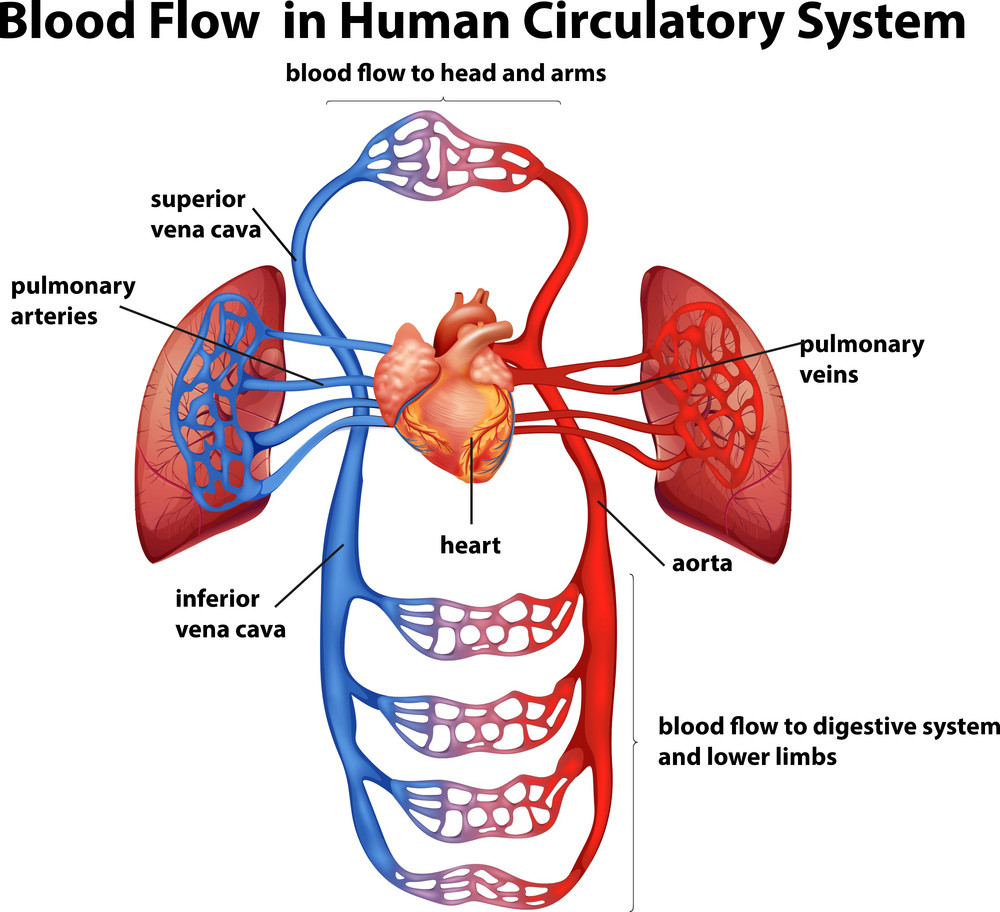 Blood pressure (BP) is the force of pressure exerted by blood in the blood vessels. BP depends on the pumping action of the heart and the amount of pressure in the blood vessels, which are in turn controlled by the autonomic nervous system. A blood vessel’s diameter changes in relationship to position of the body and the physical activity involved. When you stand up, vasoconstriction (the contraction of blood vessels) occurs in the legs.
Blood pressure (BP) is the force of pressure exerted by blood in the blood vessels. BP depends on the pumping action of the heart and the amount of pressure in the blood vessels, which are in turn controlled by the autonomic nervous system. A blood vessel’s diameter changes in relationship to position of the body and the physical activity involved. When you stand up, vasoconstriction (the contraction of blood vessels) occurs in the legs.
The nervous system controls the body’s blood pressure. An injury to the spinal cord changes blood pressure by changing the way blood flows through paralyzed limbs. In the case of paralyzed limbs, blood has a tendency to linger in the legs (pooling) and the blood pressure fails. An unusual colouration of the legs is common for people with a spinal cord injury.
An injury above the T6 can slow the pulse (BP). If your pulse falls below 50 beats per minute, you may experience dizzy spells.
Edema is caused by the absence of muscular activity and movement that would normally assist the return of blood from the limbs to the heart. Edema can occur in both the arms and the legs, depending on the level of injury.
Thrombosis and embolism are a result of poor circulation and lack of movement and stimulation to the affected limbs. When a blood clot is stationary, it is called a “thrombus”. When it becomes detached and is carried along in the bloodstream, it is called an “embolus.” In the case of a lower limb thrombosis, the affected leg may appear hot, swollen and have a reddish colour as compared to the other leg. If you suspect a thrombosis or embolism call your doctor immediately and go to your local hospital emergency.
Things to help circulation and blood flow
- Wear support hose or elastic stockings to exert pressure over the leg, supplementing the weak pressure in the veins and aiding blood circulation.
- Practice regular passive range of motion exercises while aiming for maximum range of motion.
- Change the position of your legs every 2-3 hours.
- Do not spend more than 4 hours sitting in your chair or in your bed.
- Elevate your legs while lying down. Place cushions under your legs.
- Practice bending and stretching exercises on a daily basis to the level of your capability. Always striving to achieve more.
- Practice daily exercises that will stimulate movement in your limbs to the level of your capability. Always striving to achieve more.
“Why does my blood thus muster to my heart; making both it unable for itself,
and dispossessing all my other parts of necessary fitness?”
— William Shakespeare, 'Measure for Measure'
![]()
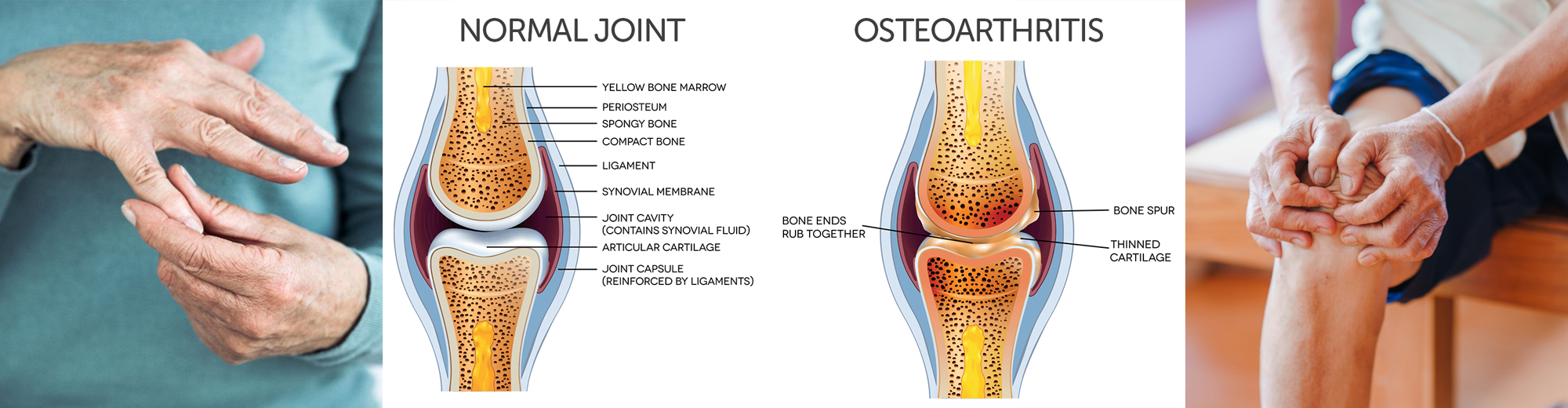
Development of osteoarthritis after an SCI
Osteoarthritis is a form of arthritis in which the cartilage covering the ends of bone wears down over time. This causes friction with neighboring bones, leading to pain and discomfort. Spinal osteoarthritis occurs in the spine, but osteoarthritis can also affect other areas, such as the hands, elbows, shoulders, knees, feet, toes, and hips. Deterioration of the bones due to lack of use after a SCI is common and the development of osteoarthritis a reality for many with a SCI.
The first-lineTrusted Source treatments for spinal osteoarthritis aim to decrease pain, increase mobility, and strengthen neighboring muscles. They can include:
- doctor prescribed medications
- over-the-counter pain medications
- supplements
- nutrition
- staying active
- strengthening exercises
- aerobic exercises
- physical therapy
- massages
- weight loss
Nutrition & Dietary Changes & Challenges
A great deal of information is covered on this website with regards to nutrition, diet, food choices. There is also a plethora of information on the internet, YouTube, and social media with regards to diets, nutrition, healthy food choices, fasting, juicing, supplements, herbals, exercise and alternative health choices.
Sexuality and Intimacy after a SCI
It doesn’t matter what level of spinal cord injury you have or whether your injury is partial or complete; you are going to experience some level of sexual dysfunction, whether you are male or female. Each person will rediscover sexuality in very different, personal ways. This is because each person has different physiological, psychological and emotional perceptions of sexuality and intimacy that they had before the injury and after the injury.

Grieving for your old sex life will weigh heavy on you as long as you have not found in your body, your heart and your present state of mind a source of love and pleasure.
For women, the ability to engage in sexual activity is impacted less than that for men with a spinal cord injury. For men the difficulty lies with achieving and maintaining an erection like they did before the SCI. Women experience inadequate lubrication and problems with arousal and achieving orgasm. For both men and women, the loss of sensation is the source of their grief and difficulty to deal with a relationship.
A psychogenic erection is when there is neurological damage below S1. The nerves to enervate the penis are damaged. No amount of stimulation will produce an erection. However, mental stimulation can provoke psychogenic erections.
Injuries between the L3 and S1, even if a complete injury, will not affect either psychogenic or reflexogenic erections. However, the erection may not last long. Between T11 and L3 an injury leads to varying degrees of loss of the psychogenic component.
With injuries above T12 the nerve impulses arising from the brain (psychogenic) cannot reach the thoracic centre, unless there is a partial injury. The pathway for psychogenic stimulation is cut off. Reflex activity at the genital level may invoke an erection, which can occur with a variety of bodily stimulation such as receiving a massage, bathing, clothing rubbing on the skin, etc.
Things to help with sexuality and intimacy
- Allow you and your partner time to get familiar with what has changed in your life.
- Allow and devote time for each other and your sexual relationship.
- Understand and practice psychogenic stimulation (non-genital) of psychic origin, meaning produced as a result of thoughts.
- Understand and practice reflexogenic stimulation (direct) which is physical stimulation of the genital organs by men or women.
- Use a lubricant.
- Engage in prolonged foreplay.
- Seek out new erogenous zones.
- Try to stimulate natural erections and arousal whenever possible.
- Engage with sexual toys; vibrators and arousal aids.
- Consult with your medical team for specific medications that can help with arousal and sexuality.
- Talk with a counsellor, a therapist, or join a group where you can talk about intimate issues.
For more help and understanding about sexuality and a spinal cord injury or any disability, I highly recommend reading the book titled: "The Ultimate Guide to Sex and Disability" featured in my reference pages.
“I can’t move my legs anymore; it’s obvious that I’m paralyzed.
Why go on?, some men think; If you are convinced you are impotent,
just thinking you are is enough to rob you of your abilities.”
— Anonymous
![]()
Obstacles to overcome after a spinal cord injury
Regaining independence after a spinal cord injury is a significant hurdle in anyone’s life, no matter what the extent of the injury. Understanding and support from family, friends, community, the medical team and the physiotherapy team is of the utmost importance and is crucial to how fast the individual has the capacity and motivation to climb the mountain that lies before them. The following is a list of obstacles that one has to overcome:
-
Attitude – overcoming the internal negative thoughts; the poor me, the why me; bitterness, anger, hatred, regrets; and so many other feelings.
-
Rehabilitation – spans many aspects from physical therapy, diet and lifestyle changes; to breathing, toileting, talking and feeding oneself; to relearning how to walk or drive a vehicle.
-
Listening to One’s Body – most of us take for granted all the things that our body does without us thinking about it. After a SCI, a person must become in tune and aware of their body on many levels. Knowing how the body feels or is reacting to a certain food, an exercise or a therapy is key to being able to manage one’s own health.
“Sometimes it takes dealing with a disability - the trauma, the relearning, the months of rehabilitation therapy - to uncover our true abilities and how we can put them to work for us in ways we may have never imagined.”
—Tammy Duckworth
![]()
Keys to Independence and Rehabilitation
-
Aids for Personal Independence
-
Wheelchair, walkers, lifts, leg braces, orthotics, knee/ankle and back braces
-
-
Home
- Mechanical lifts – indoor and outdoor
- Ramps
- Automatic door openers
- Renovations and considerations for bathing and toileting
- Modifications to kitchen cupboards and cooking area
- Doorways should be a minimum of 34” wide
-
Daily Life
- Devises that help with daily tasks such as helping with meal preparation, cleaning and washing,
- Dishwashing aids
- Assistive devices to help reach and grasp object, turn door knobs and access light switches.
- Transfer boards to help with transfers to and from a wheelchair to bed, toilet, chair, sofa and vehicles
- Adaptive aids for eating such as special tables and trays
- Aids to help with getting dressed, ironing cloths, hanging cloths and sewing machines
-
Environment
- Home automation systems indoor and outdoor to help with a multitude of tasks from controlling lights to heating the home, security systems, sprinkler systems, etc.
- Considerations for lawn and garden care, dog walking, snow removal, garbage collection, etc.
-
At Home Care
- Having an appointed care giver come to your home on a regular basis. These services are usually covered by government assistance programs. You will have to make contact either on your own or through your doctor.
- Provide assistance for your everyday needs such as bathing, getting dressed, cooking, cleaning, help with exercises, etc.
- Rehabilitation services or in-home physiotherapy or through a local facility in your local community. These facilities may have gyms, workout rooms, therapy pools and physiotherapists to help you.
- Social support, family respite and care-sitter services are provided by the government and your local communities. Take advantage of these services.
-
Transportation
- You may or may not be able to drive after a SCI. You may not be able to drive for a long period of time as a result of your rehabilitation.
- Cars, vans and mini-vans can all be adapted for people with paraplegia or quadriplegia depending on the degree of disability.
- Most communities provide taxi and special need transportation to and from your home to medical appointments, shopping, visiting friends or family. There is no extra charge for calling on these service.
- If you are disabled as a result of your SCI make sure that you get your ‘reserved parking’ sign. Application for these signs are made to the government through your doctor or medical team member.
-
Communications
- Libraries, coffee shops, schools and other organizations provide free service for the use of computers, internet and WiFi.
- On-line banking and bill paying.
- Cell phones are becoming more and more a part of everyday life for not just business but social interactions, news, and keeping up with what is going on in the world.
-
Financial Assistance
- Depending on where you live, the government programs and private funding that is available; you can apply for funding to cover or offset the cost of certain medical devices such as wheelchairs and walkers.
- Private insurance companies and non-profit foundations may offer financial assistance.
- Crowd funding.
“The road to rehabilitation and social re-integration that a person with a spinal cord injury must follow is sometimes long and strewn with pitfalls.
It’s a challenging journey, both physically and emotionally.”
— Anonymous
![]()
Source: United Spinal Cord Association
Source: North American Spinal Cord Consortium
Source: National Spine Health Foundation
Source: Scire Community, Spinal Cord Research
Source: Spinal Cord.com
Source: Spinal Cord Injury Canada
Source: Spinal Cord Injury Ontario
Source: Christopher Reeve
Source: National Institute of Neurological Disorders and Stroke
Source: National Association for Incontinence
Source: Health Care Utah
Source: Mayo Clinic
Source: Health Line
Source: Very Well Health
Source: National Library of Medicine
Source: Wikipedia
Resources: Books–Articles-Videos-Podcasts