
My Story Continues
Importance of Exercise
 It is winter here where I live. I am pretty much confined to my room as wheelchairs and snow just don’t go well together. I have been working on my exercise routine and increasing reps on my standard exercises and adding new things such as yoga poses and weights which I am using to increase my upper body strength.
It is winter here where I live. I am pretty much confined to my room as wheelchairs and snow just don’t go well together. I have been working on my exercise routine and increasing reps on my standard exercises and adding new things such as yoga poses and weights which I am using to increase my upper body strength.
I have been working out at a gym since I was 16 years old, when my mother signed me up so that she didn’t have to go on her own. After I was married, my husband and I went faithfully twice a week and then worked out at home on my own. When I moved to the farm in 2006 there were no gyms close by and just being on the farm was a workout.
Now that I am disabled and living life in a wheelchair I have come to realize how important keeping physically fit, especially having a strong upper body is. Upper body strength is the mainstay of living in a wheelchair. The ability to do transfers and be self-sufficient all depends on upper body strength.
I am now one year after my back surgery. The time that I spent at Providence Health Care doing physiotherapy was the absolute best experience and it served to inspire me to get into doing my own physical therapy exercise routine when I got home. The worst setback was the effects of the chemotherapy (Melfalin) that went along with my stem cell transplant, which resulted in about six months to get my immune system and physical body back to where it was prior to that experience.
Now I am in a much happier place. My body has been responding very well to the exercise routine that I have created for myself. I have increased the number of reps on many of my regular exercises and with the help of these three wonderful books I have added quite a number of additional exercises to help with flexibility, upper body strength, back and abdominals. I have also added a yoga routine to my workout. My annoying bloated belly is actually going down and becoming much firmer.
In pushing myself and trying to develop a more intense routine, I have strained my back a number of times, which means that I have to take it easy the next day or not do exercises at all. It doesn’t take long for my back to come back, which to me means that my muscles are responding to the workouts.
I have been doing some standing exercises using my stationary walker and my wheelchair. These are going well, but the progress is slow. I am finding that my left side of my body is not as strong or as responsive as my right, but at least it is doing its best to keep up.
 Kathryn
Kathryn
1 Year Anniversary after Cancer Diagnosis & Spinal Cord Injury
 Wow, it has been one year to the date from my admission to the hospital where they found a cancerous tumor on my spine which caused me to be paralysed from the breastplate or T4 down to my toes.
Wow, it has been one year to the date from my admission to the hospital where they found a cancerous tumor on my spine which caused me to be paralysed from the breastplate or T4 down to my toes.
I spent 9 out of 12 months in a hospital going through all kinds of tests, treatments and physical therapy. The worst of which was the Melfalin chemotherapy that was given to me prior to stem cell transplant. That whole experience was like dying and then being resurrected. It was a total poisoning of my body, to which I believe I am still recovering from.
Other than that, the past six months have been an ongoing struggle to replenish my immune system and get it back up to where it was before all this happened. My son is feeding me good healthy meals. I have eliminated sugar, coffee and alcohol and don’t miss any of them. I have found a great mushroom coffee substitute for those days when I need something warm in my belly. My son has a source for local unpasteurized honey which I have in very small amounts.
Exercising is my real source of inspiration over these winter months of confinement. I am up to 30 reps on each of my exercises and have added weights for different exercises. I am working hard on my abs trying to reduce this bloated belly that I have acquired as a result of the damage to my thoarasic spinal cord. I am hoping to be able to do some exercise video with the help of my granddaughter once I give a little more time for my hair to grow back in, get a little stronger and get these weight exercises down pat. I have also started doing some standing exercises with my walker. They are challenging and I have to be careful not to strain my back. I have a bad habit of pushing myself a bit too hard. I use my OlyLife-P90 everyday and I drink my Kangen alkaline water.
The swelling and bloating in my body is dissipating. I can wear my rings again. My belly bloat is starting to go down. It is going to take a lot of exercise to get my belly back to where it once was, if it ever goes back to what I would call my normal. Apparently with a thoracic spinal cord injury as mine, when the spinal cord becomes damaged, the belly, all that makes up the abdomen blow out or as it is described, the muscles give out and everything goes loose. As a result of this there is also damage to the bowels and the bladder. With an injury such as this most of us spinal cord injury persons choose to stay close to home, close to a washroom. Sad but true, that is the nuts and bolts of my life now.
Piper, my dog brings me comfort and joy while I am confined to my room over the winter months. It is not easy for me to get outside or get out and about. My daughter and my son are very good and doing my shopping and Amazon has become my best friend for just about everything that I could possibly need other than food.
I have totally become enthralled in reading some incredibly entertaining and excising novels. My daughter and granddaughter and I are engulfed in reading several trilogies. My son is busy making his crafts, which he devotes a lot of his winter down time to doing. I will get back into doing crafts as well very soon, once I can put this book down. We had our first calf born on January 4th here on the farm. He had a bit of a hard start to life but is doing wonderfully well, growing strong on mother’s milk. We should have about 9 more calves sometime over the next few months.
I am still working with my alternative health practitioners and taking their advice for various supplements, homeopathy and herbals. I have been trying to get my oncologist to take an interest in what I am taking and doing outside of his treatments but he has been disinterested until of late when my bloodwork came back indicating that I had elevated liver enzymes. I finally gave me his email so that I could send him my list of supplements. He sent it off to the hospital pharmacist and I have made their recommended adjustments. It is nice when things come together.
 Kathryn
Kathryn
Month Five - December 2024 Update
It is month five after my stem cell replacement therapy has seen me more back to normal. I saw my spinal cord doctor at Providence Health Care Hospital in Kingston which was positive. The intern talked with me and my daughter extensively for a good hour and took notes which were relayed to my doctor who did an examination of my nerve responses. Her conclusion was that regardless of all my ups and downs over the past six months since she did a throughout exam—I am back to where I was six months ago, therefore I have reached my normal in her opinion. I will stress that that is her opinion as I am still determined to repair my nerve damage to the point where I able to walk to some level.
A week later, I had my monthly appointment with my oncologist who informed me that my multiple myeloma cancer is officially in remission. My bloodwork for my liver came back indicating that there is no more issues. We had a discussion about taking lenalidomide as a remission therapy. I questioned the dosage and he agreed to lower his recommendation from 10mg to 5mg, with the option that I can discontinue at any time or reduce the dosage to 2.5mg which would be the lowest. I have agreed to take the 5mg dosage for one month and see how it goes.
I have agreed to taking this medication despite all me alternative health practitioners recommendations as none of them are oncologists and none of them are willing to work with me closely and walk with me. None of them know the correct dosages for alternatives such as Fenbendazole or Ivermectin or any of the many other alternative options. This is disappointing, but I respect each of them for their inputs and the help and guidance that they have given me to date. I am therefore on my own to research and nail down my own personal cancer recipe. Reminding myself that I also have to deal with a spinal cord injury.
On that note, there are a number of things that continue to affect my overall health, which my oncologist says are all related to my spinal cord injury. My spinal cord injury doctor says they are cancer related—so, once again, I am left on my own to diagnose and treat myself. I am experiencing severe pain and stiffness in my hands, especially my right hand, with the symptoms being the worst at night, starting in the evenings around 8pm. I don’t understand these evening and night-time effects on my feet, especially my toes and feet are also worse at night. My daughter says that I have arthritis. Perhaps, but my instinct is saying no. I have a toe and a finger that become gnarled at night. I will have to research and investigate these conditions in more depth.
This has been a great month as far as my exercises go. I had a visit from a wonderful young lady who teaches yoga. She gave me a few more exercises to add to my morning routine. I am back to incorporating weights into my exercises.
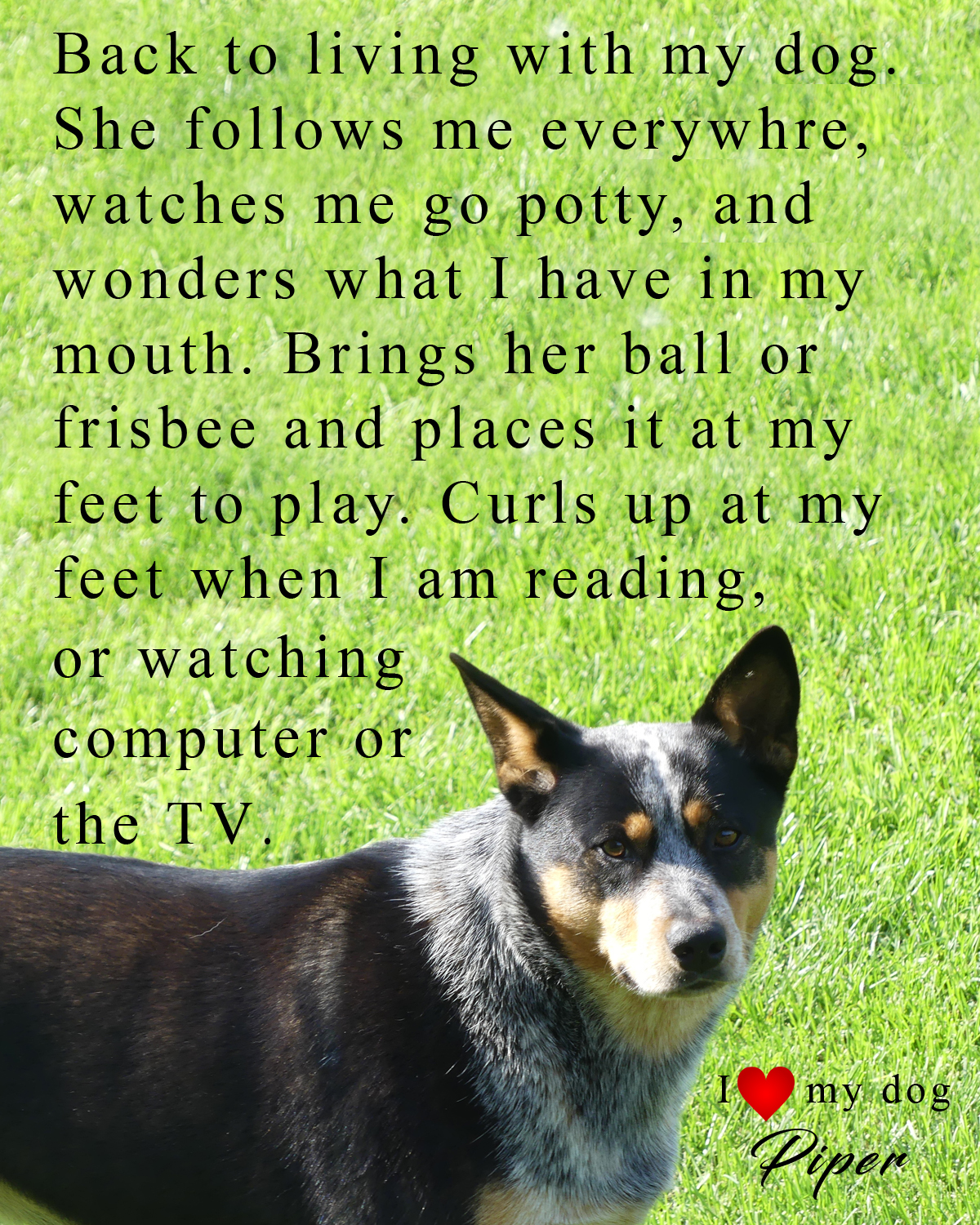 Now that winter is upon us, my dog is staying inside more. We play fetch and tug-o-war and cuddle, which is all reinforcing the relationship that we had before I went into the hospital. Since I live on a farm, my dog was forced to stay outside all the time during my stay in the hospital as nobody wanted the bother of her. She is an Australian Cattle Dog, otherwise known as a Blue Heeler, which is an extremely high energy, high strung, intense and demanding breed. I understand that she slept underneath my deck while I was away in the hospital most of 2024 (7 out of 9 months). Every day we are re-establishing our relationship which gives us both a lot of joy.
Now that winter is upon us, my dog is staying inside more. We play fetch and tug-o-war and cuddle, which is all reinforcing the relationship that we had before I went into the hospital. Since I live on a farm, my dog was forced to stay outside all the time during my stay in the hospital as nobody wanted the bother of her. She is an Australian Cattle Dog, otherwise known as a Blue Heeler, which is an extremely high energy, high strung, intense and demanding breed. I understand that she slept underneath my deck while I was away in the hospital most of 2024 (7 out of 9 months). Every day we are re-establishing our relationship which gives us both a lot of joy.
My son had his one week away from the farm to visit his daughter in the United States. We all faired okay without him. I missed the wonderful smoothies that he has been bringing me every morning. My daughter and my granddaughters kicked in to look after the cows, put wood in the outdoor furnace and shovel snow.
Christmas is coming soon. Since I cannot drive and get out shopping—I am relying on Amazon.ca which is not a company that I wish to support, but they do have everything that I need and delivery is very fast and no charge, so why would I not use them. I am crafting a few presents this year to put under the tree. I am looking forward to 2025 and putting 2024 behind me.
 Kathryn
Kathryn
Looking Back and the Reasons Why?
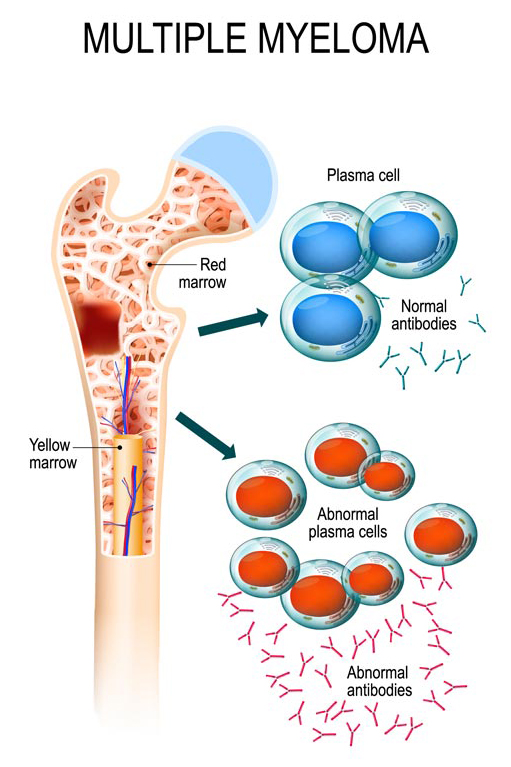 Multiple myeloma is an incurable blood cancer; also known as Kahler’s disease which is a cancer of the plasma cells, a type of white blood cells in the bone marrow. Multiple myeloma fools the body into thinking cancerous cells are normal plasma cells, and thus the cancer multiplies for years unchecked. If untreated, multiple myeloma attacks the bones, immune system, kidneys, red and white blood cells. Early and ongoing symptoms of multiple myeloma are anaemia. Multiple myeloma remains a relatively rare cancer.
Multiple myeloma is an incurable blood cancer; also known as Kahler’s disease which is a cancer of the plasma cells, a type of white blood cells in the bone marrow. Multiple myeloma fools the body into thinking cancerous cells are normal plasma cells, and thus the cancer multiplies for years unchecked. If untreated, multiple myeloma attacks the bones, immune system, kidneys, red and white blood cells. Early and ongoing symptoms of multiple myeloma are anaemia. Multiple myeloma remains a relatively rare cancer.
The causes of multiple myeloma are not clear. Research suggests, like many other cancers, can be related to exposure to toxic chemicals, herbicides, pesticides, lack of certain nutrients in the diet, toxic foods and unclean water. There is a close correlation between multiple myeloma and a condition called ‘monoclonal gammopathy’ or MGUS where there is an excess of protein molecules, called immunoglobulins in the blood.
Somewhere back in time I must have experienced a genetic mutation that my body didn’t self-correct. The mutation became my body’s new normal and myeloma cells replicated unabated. To date there is no cure for multiple myeloma, but it is treatable and highly manageable which is encouraging. Survival rates are anywhere from 2 to 5 years depending on what stage the cancer was at when diagnosed. There are many people with multiple myeloma that continue to survive 10 to 12 years or more. Personally, it is my intention to survive as long as I possibly can. Every day is a new day.
“You have to be willing to give up the life you planned, and instead,
greet the life that is waiting for you.”
— Joseph Campbell
When I look back at my life and ask the question—why me—how did this cancer infiltrate my body and why didn’t it get diagnosed sooner? Many questions.
First off, I worked in corporate administration all my working life; exposed to fluorescent lighting and all of the businesses that I worked for were also manufacturing facilities which used chemicals and toxic substances that we as employees where subject to either physically or airborne through the ventilation systems. Why did I get cancer and the people I worked with did not?
Second, I grew up with parents that were very much into gardening. They used fertilizers and I helped them with the lawns and gardens and then adapted their methods into my life for a period of at least 30 years until my son introduced me to organic, biodynamic and permaculture agricultural and gardening practices. Thus, for the past 20 years I have lived a life eating and growing organic foods. Again, I ask the question, why did I get cancer?
Looking at my diet, however, working in the environment that I did, I adopted the habit of consuming many cups of coffee over the course of the day, eating and drinking at my desk. I have to admit, my diet for most of my life up until the past 18-20 years has not been the healthiest, but it was better than the average household. My father was a smoker and a heavy drinker. Growing up in an era where cigarette smoking was considered fashionable and normal, it was difficult to not be exposed. However, I never smoked, but I did consume alcohol as it too was the normal. My parents were heavy social drinkers and when entertaining it was normal to have several bottles of wine on the table, beer or other alcoholic beverages for before and after meals.
 So, I still have still not figured out where or how this cancer infiltrated my body. In 2017 I fell off a ladder and broke my right femur bone just above the knee. The surgeon, who set my leg, told me that that x-rays and what he saw in surgery, indicated that I was in the beginning stages of osteoporosis, which is another one of those silent diseases that is characterized by weak, brittle and porous bones. My GP (General Practitioner or Family Doctor) sent me for bloodwork and a bone density test which came back confirming the initial signs of osteoporosis. The bloodwork showed some concern over one of my kidneys, however, second blood test shows no concerns. We agreed to follow up every two years. It is my belief, to this day, that had my GP at the time done a deep dive and ordered more extensive blood tests that the early stages of multiple myeloma would have been identified. Had that been the case, the myeloma would have been Stage 1 and completely treatable.
So, I still have still not figured out where or how this cancer infiltrated my body. In 2017 I fell off a ladder and broke my right femur bone just above the knee. The surgeon, who set my leg, told me that that x-rays and what he saw in surgery, indicated that I was in the beginning stages of osteoporosis, which is another one of those silent diseases that is characterized by weak, brittle and porous bones. My GP (General Practitioner or Family Doctor) sent me for bloodwork and a bone density test which came back confirming the initial signs of osteoporosis. The bloodwork showed some concern over one of my kidneys, however, second blood test shows no concerns. We agreed to follow up every two years. It is my belief, to this day, that had my GP at the time done a deep dive and ordered more extensive blood tests that the early stages of multiple myeloma would have been identified. Had that been the case, the myeloma would have been Stage 1 and completely treatable.
This leads me to where I am today. In my personal story, I indicated that I experienced severe pain in my right shoulder that migrated to my spine and within two months I was admitted to the hospital for emergency surgery to remove a tumor from my spine that was the size of my thumb that consumed my T4 to T6 and blocked the spinal fluid from flowing. Had my GP at the time sent me for an MRI or CT-Scan; the tumor would have been identified and I would more than likely not be paralyzed and living my life in a wheelchair. All the shoulda-woulda-coulda’s don’t count! What is–is what it is! I cannot go back in time and change things. I can only go forward from here.
I have always been attracted to alternative health. I have worked with numerous alternative health practitioners over the years. I have worked with reiki and have a masters degree in reiki myself. For well over 30 years of my life I have worked out in a gym twice a week, practiced yoga, gi-gong, tai-chi as well as creative dance. All throughout the covid years, I only came down with covid once. I have had the usual spring and fall cold or flu and I have been exposed to my grandchildren’s ongoing illnesses that they bring home from school with no adversity. My immune system has been strong and healthy by all indications. For the past year, I have spent 7 out of 9 months on my back in the hospital and not once did I get covid, a cold or any type of viral or bacterial infection. During that time, I did not take any vitamin supplements, only what the hospital allowed, which was only vitamin D and a calcium pill daily. I went back on my daily supplement regain after I was discharged home. I feel that I remain healthy to this day as far as my immune system goes.
There is so much with regards to current health care system that frustrates me and that I just cannot get my head wrapped around. One of the most frustrating things I experienced with doctors and nurses in the hospital was being treated like someone that is not supposed to know. I would ask a question and simply getting a blank stare or a change of the subject. It was as if they all went to school or had a course on how to deal with patients. I found that I got more answers and more honesty from the PSA’s, transporters and maintenance people. I feel that the medical system is under obligation to promote and administer chemotherapy, radiation and surgery as the only treatment for cancer when there are many alternatives plus supplements that they won’t consider because they under obligation to the system that pays their salaries. Forgive me if I am wrong.
I am a digger, a researcher and I have read many books, watched many videos and have done my share of internet browsing. I have made it a passion of mine to be educated and knowledgeable about everything that crosses my path. This is who I am; I have created this website to help others on their journey; may it be cancer or a spinal cord injury or a chronic illness or a disability.
 Over the past year, I have met many people with many different types of cancer and I have met many people experiencing a disability for the first time. I have listened to their personal stories, felt their pains, their frustrations with the medical system and their uncertainties about the future. I realize that I need to be grateful for my life as it is, as things could be far much worse than they are. I have a wonderful family and support group that are there me for which I am extremely grateful for. If there was ever any blame to be placed upon anyone or anything in my life that may have contributed to me being where I am, I offer forgiveness from my heart. Hoʻoponopono!
Over the past year, I have met many people with many different types of cancer and I have met many people experiencing a disability for the first time. I have listened to their personal stories, felt their pains, their frustrations with the medical system and their uncertainties about the future. I realize that I need to be grateful for my life as it is, as things could be far much worse than they are. I have a wonderful family and support group that are there me for which I am extremely grateful for. If there was ever any blame to be placed upon anyone or anything in my life that may have contributed to me being where I am, I offer forgiveness from my heart. Hoʻoponopono!
“Yesterday is history, tomorrow is a mystery, but today is a gift
– that’s why it’s called ‘the present.”
— Eleanor Roosevelt
Kathryn 
Month Three After Stem Cell Treatment
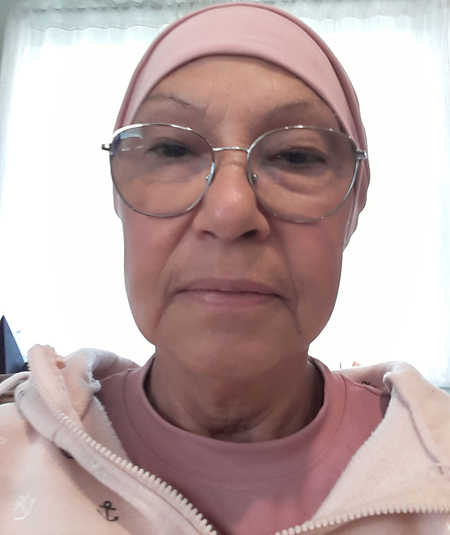
 Hurray, my hair is finally starting to grow in!
Hurray, my hair is finally starting to grow in!
So here I am in month three after my stem cell treatment. I can honestly say that I am not overly happy with the medical system. I am grateful that I live in Canada and I have free medical care, however, the quality of care is questionable. My oncology doctor is still being elusive with regards to my blood work results. When I ask him for a copy of my blood work, he says he will have to have his secretary mail it to me, then I have to follow up with her to make sure that is going to happen. He is still pestering me to consent to taking the low dose lenalidomide treatment as a maintenance program. I told him that I want to know exactly where my cancer stands before I make a decision.
Back in April, my oncologist from Kingston Hospital told me that my monoclonal proteins (which indicate multiple myeloma) has decreased from 48.1 g/L in January to 17.9 g/L in March 2024. I said that to my knowledge this test has not been updated. He said, “Oh, yes, it was done in August”, and he quickly went out of the room and came back in with a copy of the report. I showed that monoclonal proteins had dropped from 60.0 g/L in February to 4.0 g/L in August. He indicated that these tests will be done every three months. So I told him that we were obviously due for a new test. He said, yes, yes, I will put in a requisition. I asked, so can it be done today while I am at the hospital since I live far away. He hummed and hawed and then said that yes, he would take care of that. I asked him to make sure he sent me a copy of the report as I know not to ask him for a copy when I am in the room with him. He assured me this would happen. Two weeks later and I still do not have a copy. I am having to call up his office and remind his secretary once again. Then he comes back to the lenalidomide issues and again, I told him that I wanted to wait and see exactly where my cancer is.
As for month three in general, it has again been a difficult month. The neuropathy in my legs is still the same. I am now having numbness in my right thumb and stiffness in the joints on this hand as well as I am experiencing excruciating hot pain during the night. I don’t think this is carpal tunnel syndrome as one doctor suspected. My left hand is also showing signs of numbness and stiffness. My daughter suspects arthritis due to my age. I am not ruling out that there might be additional damage to my spinal cord that is causing this. I finally have an appointment with the spinal cord injury doctor from Providence Health Care Hospital in Kingston mid-November. I can’t wait, as I will have a lot of questions for her.
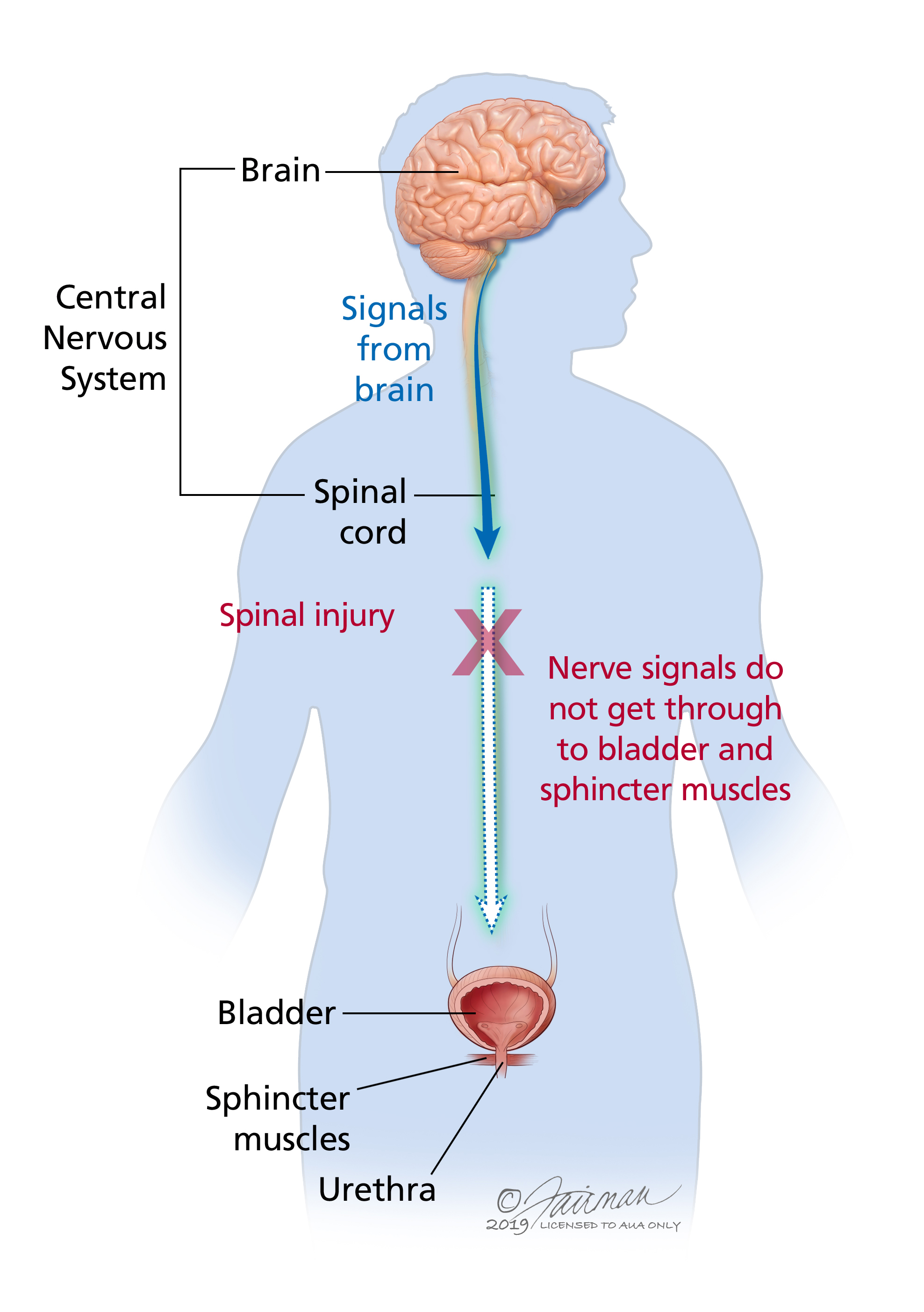
The other thing that I am experiencing is increased incontinence. Is this from the chemotherapy or is this a result of something that is going on in my spine, such as a compressed disk or active lesions? My back has been sore and is slightly painful come night-time. Makes me concerned as to what is going on.
My new family doctor stopped by my house to drop off some paperwork. Amazing that she is willing and wanting to make house calls, especially since she know that I am isolated, in a wheelchair and without someone to drive me to appointments unless it is convenient for them.
She did explain to me about the belly-bloat that I experienced with the onset of the tumor/cancer/spinal cord injury. She said that when a spinal cord injury such as mine occurs in the upper thoracic are of the spine, it cuts off the signal from the brain to the organs below that point of injury. Okay, how come I see some people with a bloated belly and others without. She only commented that everyone is different. I am doing my exercises faithfully every day and working on my abdominals. The belly is tightening, but still distended.
I had full continence after my surgery up until July when I went into the hospital for my stem cell treatment. Everything has gone to pot since then (literally). I can’t think that this increased incontinence is not a result of the chemotherapy. The more and more I think about things, the more and more my mind is made up not to take the lenalidomide.
Kathryn 
Month Two After Stem Cell Treatment
 My first appointment with my oncologist after the stem cell replacement treatment was mid-August. It was simply weigh in, bloodwork and a quick review. Everything looks good and he wanted me to agree to taking the Lenalidomide chemotherapy pill as a maintenance a.s.a.p. I told him I would think about it. More research to be done on this subject before I make a decision.
My first appointment with my oncologist after the stem cell replacement treatment was mid-August. It was simply weigh in, bloodwork and a quick review. Everything looks good and he wanted me to agree to taking the Lenalidomide chemotherapy pill as a maintenance a.s.a.p. I told him I would think about it. More research to be done on this subject before I make a decision.
Day by day my strength is coming back. I have started taking a heavy regime of vitamin supplements to get my immune system back up to where it was before the chemotherapy. I have been reading a lot of books and doing a lot of internet research on many topics. I not only have cancer, but I also have a spinal cord injury that goes along with it to consider.
By the end of August, I was able to do 20 minutes on my special exercise bike which is ideal for me to pull up to on my wheelchair and peddle. Unfortunately, I have to wait for someone to be available to lock my feet in and take me off when I am done. I usually wait for my granddaughter to come home from school and put me on the machine. By mid-September, I have graduated to 25 minutes at which time my legs start to shake with neuropathy, so that is my current limit. At the end of September, I have increased the tension and graduated to 30 minutes.
I have added small weights to legs and arms which I am incorporating into my daily bed exercises. I have setbacks where I have to pull back on the weights. Some days the exercises cause me fatigue.
I think the biggest disappointment that I have had this month is with the neuropathy in my legs. It has gotten better at night since I added glucosamine to my supplement regime. During the day, especially after I have had a good exercise routine workout, my legs feel swollen with the neuropathy. Nothing I do seems to relax them, not even resting in bed.
My hair is just starting to grow back. There is a little fuzz appearing on my bald head. I have had perfect teeth all my life. Almost no cavities. I am still having boughts of incontinence that has been happening since the stem cell replacement. With aging, I have had receding gums, however, after the stem cell treatment and that large dose of chemotherapy (Melfalin), I have noticed that my gums are receding more and they are very sensitive. My teeth are becoming more yellow/grey as opposed to white. I researched the effects of chemotherapy on teeth and I am experiencing exactly what is to be expected. I wish more of these after/side effects would have been discussed with me by the oncology team. I will refer to it as a team, as the medical system bounces you around from one person to another, I believe this is done so that nobody gets attached to the patient and they can cover up their inconsistencies and mistakes.
On a positive note, I am very excited that I have found a used Batec Mini wheelchair power-drive. I have not got it yet. It is very expensive even as a used piece of equipment. This device will allow me to go across the grass and along the gravel laneway. I will be able to get out to the barn, the greenhouse, visit the cows and play with my dog. I am very excited about this. Will keep you posted.
Kathryn 
First Month after Stem Cell Replacement
First Month after Stem Cell Replacement
 Being in the hospital for a whole month on my back, not able to even get up to go to the toilet, bathing, eating and just having a sense of being alive was the most terrible experience of my lifetime. The nausea was overwhelming. I could not put food to my mouth, let alone swallow.
Being in the hospital for a whole month on my back, not able to even get up to go to the toilet, bathing, eating and just having a sense of being alive was the most terrible experience of my lifetime. The nausea was overwhelming. I could not put food to my mouth, let alone swallow.
The stem cell replacement treatment was not what I expected. I cannot get my head wrapped around the process and the heavy dose of chemotherapy that was delivered into my body and then my reasonably healthy stem cells were re-introduced into that toxic environment. The effects of the chemotherapy on my body were devastating. The most devastating was the loss of my hair and the incredible fatigue.
Throughout the month of July when I was hospitalized, I followed my daily bloodwork levels, my neutrophils and other key elements as they all went down to 0.0 and then started to come back up. When I was released from the hospital, my levels were still below the ideal markers. Not one single one of my many doctors came to see me in the hospital. The group of nurses that orchestrated the stem cell process did not check in on me.
I was looked after by the nurses, PSA’s and the doctor on call for the floor. Asking questions got me nothing but blank stares. There were a few of the nurses that gave me my blood numbers and neutrophils, but little explanation about what anything meant. They really wanted me out of there, home, and threatened that if I did not start eating solid foods they would start tube feeding me. They tried, but that did not work. I finally ate some solid foods and the next day I was discharged.
The first thing that I did upon coming home was to purchase a Kangen alkaline water machine. I have been doing a lot of research on how alkalizing the body through food, water and diet can have a lot to do with battling cancer, building up and balancing the immune system. Refer to some of my book reviews.
The other thing that I am doing to help with my battle against multiple myeloma is to spend 20 to 40 minutes, twice a day, on a PEMF machine that a very good friend has loaned me until I can purchase one for myself. At first I didn’t notice anything, but after using it faithfully for one month, I can sense that it is doing something with my body. The neuropathy that I experience in my feet, legs and abdomen seems to calm down. I like to use the machine after dinner before going to bed.
The neuropathy in my feet, legs and abdomen is very painful during the night but is quite tolerable during the day. As soon as the dark comes on at night, I can feel my body stiffen and then the pain and discomfort increases. It is very concerning during the night if I have to get up to go to the toilet as my legs are weaker and transferring from my bed to the wheelchair to the toilet has to be very carefully executed. As daylight comes through my bedroom window at daybreak, all this neuropathy dissipates.
The first two weeks of being home after my stem cell replacement treatment were very difficult. I lost all muscle tone throughout my body. My legs were useless and my upper body strength was gone. I had to depend on my daughter and my son to help me in and out of bed, my wheelchair and to the toilet. I slept most of the time during these first few weeks as the fatigue, like in the hospital, was overwhelming. Thank goodness for being home and being able to eat healthy food that we grow on our farm instead of hospital food.
Moving into week three of being home, my legs are starting to get stronger. I am starting back into my daily bed exercise routine, which are mostly stretching and gentle muscle exercises. My body is calling for movement. Movement seems to help with the neuropathy. I am spending more time in my wheelchair and getting outside for fresh air.
I had my first appointment with my oncologist/hematologist doctor at the 3 week mark. He did bloodwork, but did not discuss it with me. He went straight to further chemotherapy treatments and going on Lenalidomide as a maintenance program, which is a pill that I would be taking daily for an indefinite period of time. I am going to have to research and sit with this decision. I told him that I was never going to do another stem cell replacement. It was just to much!
Kathryn 
Going into My Stem Cell Replacement
 I am excited in a way to do this stem cell replacement treatment. All the doctors and nurses have been touting the benefits of this treatment for multiple myeloma. The research that I have found on the internet says the same thing, mind you, pretty much all of the internet content is mainstream, universities and hospitals that are paid to go along with the government narratives. (My opinion).
I am excited in a way to do this stem cell replacement treatment. All the doctors and nurses have been touting the benefits of this treatment for multiple myeloma. The research that I have found on the internet says the same thing, mind you, pretty much all of the internet content is mainstream, universities and hospitals that are paid to go along with the government narratives. (My opinion).
The week before being admitted, I went for bloodwork and a pre-evaluation to make sure that I still qualified and that my numbers (whatever they might be) were all in line with what they wanted to see. I never got a report on this bloodwork.
I explained to the admitting nurse that ever since May I have been experiencing extreme ups and downs with my bowels. I either have diarrhea or constipation. My bowels feel irritated and bloated. Not good. She told me point blank, “Don’t worry about your bowels, we are going to give you more diarrhea and more constipation and you will be going home with it”. I didn’t expect that, however, I was told that everything would be okay and I would probably breeze through it all because I was generally healthy and fit. I had to wait in the hospital for my bloodwork to come back from the lab and then I was excused to go home.
The following week I arrived at the hospital. I was admitted and put in a shared room with another woman. This was a good sign, as many of my hospital roommates over the months have been men. Men and women should not be cohabitating in hospital rooms for many reasons. This arrangement lasted but one day as the woman could not handle my wheelchair and how I had to manoeuvre in the washroom. I was then moved to another room with a very nice older woman who also had multiple myeloma and was in for her third stem cell treatment. She told me this would be her last as the other two did not take. She had come to term with death and we had wonderful conversations about death and dying during our stay together.
 On day two, I was escorted down the hall to the room with the stem cell collection equipment where my stem cells that had come back from storage in Ottawa, would be placed back into my body. The team was very pleasant and explained everything every step of the way. It was a totally painless operation. Because my stem cells were stored in liquid nitrogen, they felt slightly cold going into my body, but quickly warmed up once in my veins.
On day two, I was escorted down the hall to the room with the stem cell collection equipment where my stem cells that had come back from storage in Ottawa, would be placed back into my body. The team was very pleasant and explained everything every step of the way. It was a totally painless operation. Because my stem cells were stored in liquid nitrogen, they felt slightly cold going into my body, but quickly warmed up once in my veins.
Each day that I was in the hospital, I was given an injection of “Grastofil” which was to help my stem cells multiply once they were back in my body. I asked again about my hair falling out and the reply that I got was; “not everybody loses their hair”. That was reassuring!
On day four, I was given a small bag of “Melfalin” which is a high dose chemotherapy drug used for blood/bone cancers such as multiple myeloma. Day four and five, I had no reaction, but then on day six it kicked in, my neutrophils started to decline and I was moved into isolation for the remainder of my stay in the hospital.
Two days after receiving the Melfalin, my hair all fell out. Not happy!
My neutrophils continued to decline until they bottomed out at 0.00 which meant that I no longer had an immune system. The nausea quickly set in and I became terribly weak, unable to get out of bed to go to the toilet. I was back on the bedpan and curled up in the fatal position in bed for the remainder of my stay. Food became tasteless and it was difficult to swallow, not that my throat was thick, but the taste and smell of food was repugnant. Dry heaves were common. Eventually I could not swallow oral medication and they put me on IV fluids and IV medication. This was ideal for me as I just laid in bed and slept the days and nights away.
I ended up staying longer than my 30 day time limit and they wanted me to start eating solid foods, but that was just not possible. They finally gave me an ultimatum to eat or they would put a tube up my nose, which they even tried, but I had to push them away. I finally consented to eating something, anything, and the next day I was discharged. I was discharged with my neutrophils just above 0.00. I did not feel good about this. II was also very disappointed that not one of my oncologist or the stem cell team came to see me during my stay. I only saw the doctor on call for the floor and that was for less than 2 minutes a visit to just say hi, hello, how are you, good-bye.
Needless to say, this was not a good experience and I went home feeling totally unsupported and not knowing where my cancer was, let alone my overall health and immune system. I would not recommend this treatment to anyone unless you have thought long and hard. In the end I felt like I was sold a vacuum cleaner that I didn’t need from a pushy salesperson.
Kathryn 
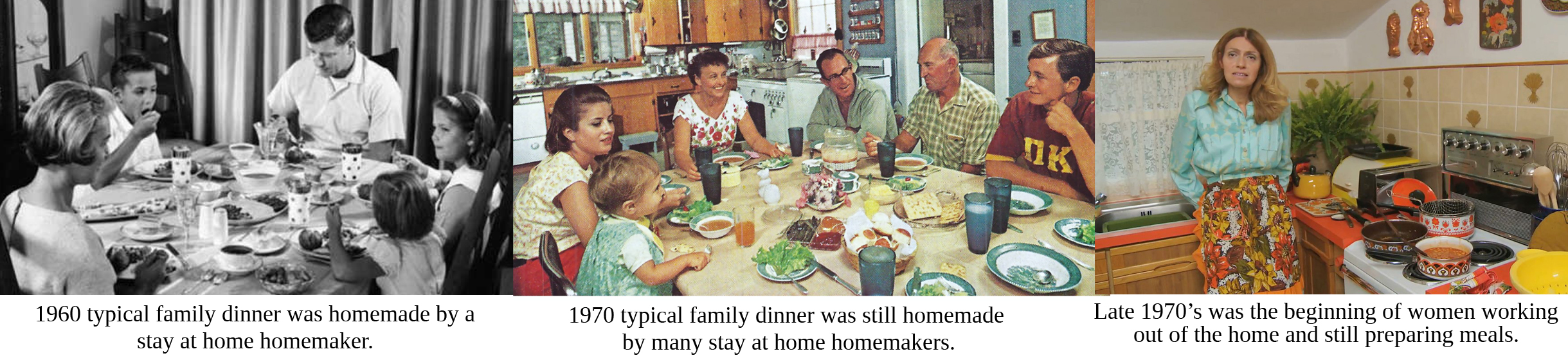
Are Poor Eating Habits Generational?
I must say, yes. Yes, I have been caught up in the generational wheel. I was raised in the 1960’s to 1980’s. Despite the fact that both my parents were raised on farms, their attitude towards farming was that it was a poor man’s lifestyle. They did not consider the quality of the food that they grew up with. My mother aspired to work outside the home. She did not want or desire to be a stay at home mother. She hated cooking and thus she cooked to live instead of living to cook. We grew up on quick meals, and junk food. My parents loved to entertain, so whenever they entertained the food flowed–steak, potatoes, vegetables, salads and alcohol. When I got married and started raising my own family, I inherited many of those traits, especially when it came to food. I did not live to cook, I cooked to live. I in turn fed my family grocery store discounted food, fast foods, and easy to cook meals.
In 2006, my son and I moved to our organic farm and started a lifestyle of being health conscious, paying attention to what we ate and where it came from. Unfortunately, for me, the damage to my health was done as a result of my childhood upbringing and the habits that I had developed over the years. Now I am faced with cancer. When I look at all the cancer diets and recommendations for nutritional and lifestyle changes, I don’t have to make many changes for my current condition. I just need to knuckle down more and get real serious about all aspects of my life. I invite you to join me on this journey to health and well-being starting here with food and nutrition.
Kathryn 
What is Para-Belly?
 When I woke up after my spinal cord injury, my belly was bloated. I asked what happened and I got no tangible answers. I had a very hard, washboard stomach with strong abs—this was not my body! What I was told was that I had para-belly which is common among spinal cord injury victims, especially when the thoracic spine has been affected. Apparently 'para-belly' is an abbreviation for paraplegic belly.
When I woke up after my spinal cord injury, my belly was bloated. I asked what happened and I got no tangible answers. I had a very hard, washboard stomach with strong abs—this was not my body! What I was told was that I had para-belly which is common among spinal cord injury victims, especially when the thoracic spine has been affected. Apparently 'para-belly' is an abbreviation for paraplegic belly.
To this day, I have not found an answer to this question. From my own personal experience; whatever happened at the time of my SCI, the injury affected my bladder and my bowel functions and thus the belly bloat. I was able to finally talk to my new family doctor and all she could explain to me was that when there is an injury to the thoracic spine everything below the area of injury is affected and most times that affects the bowels and bladder. Many people not only have the belly bloat but have serious issues with toileting including having to do manual stimulation to both the bladder and the bowels on a regular basis as well as suppositories, enemas, and self-catheterization. It is a result of the brain being no longer able to talk to these organs. So how do they function? Something called sympathetic and para-sympathetic responses. This results in what is called neurogenic bladder or neurogenic bowels, which I discuss in more detail on my cancer page.
 I will continue to research this topic as I am still not happy with my research. If you have anything you wish to comment on or share, please do.
I will continue to research this topic as I am still not happy with my research. If you have anything you wish to comment on or share, please do.
I do know from watching videos and doing my own research that a washboard abdomen can be achieved after a spinal cord injury with a lot of exercise, patience and time. See my page on exercise for exercises to help strengthen abdominal muscles.
With ongoing research, I was able to find the following article which indicates that what I am referring to as para-belly or belly bloat after a spinal cord injury is referred to as 'upper gastrointestinal dysmotility' which is described in detail.
CLICK HERE for the full article.
The following article discusses the subject of gastrointestinal dysfunction after a spinal cord injury which leads to para-belly or belly bloat and a number of other gastrointestinal issues, which unfortunately are a life-long disfunction of the body due to the SCI.
CLICK HERE for the full article.
Kathryn 
Testimonial to Providence Spinal Cord Rehabilitation
I spent seven weeks at Providence Health Care facility in Kingston, Ontario from March 21 to May 12, 2024. It was and still remains the best experience of my 7 out of 9 months in hospital institutions this past year.

Upon being admitted to PHC, I was greeted by a barrage of friendly faces of nurses, PSW’s, PSA’s, students and doctors. I was assigned two physiotherapists, one for my actual physiotherapy and the other which would also provide physiotherapy but their focus would be more getting me back home into an environment that would work for me. They would assist me with various ways to transfer to and from my wheelchair, getting me properly fitted for the ideal wheelchair and helping me to order that ideal wheelchair. We practiced transfers to and from a mock up vehicle that could be programmed to the height of my vehicles. We practiced transfers to and from the toilet, the bed and we went outdoors and practiced going across grass, up and down ramps and across gravel with my wheelchair.
My day started out by waking up around 6:30am, getting dressed and then doing stretching exercises in my bed. Breakfast was served between 7:30am and 8:00am. I would then go down the hall and do an upper body workout on the arm machine and then do a couple laps down the hall to the cafeteria and back in my wheelchair. Morning therapy session was from 10am to 11am. Lunch was as 12 noon in the common room. Another physiotherapy session in the afternoon from 2pm to 3pm followed by dinner at 6pm back in my room. More laps up and down the halls and free time to read, meditate or nap in my room. Lights out or bedtime was on our own. Evenings could be spent socializing with the group that would come together by the nurses station, do laundry and watch TV in the common room or in my own private room.
One of the therapies that I looked forward to was time in the heated, salt water therapy pool. Two to three times a week with my therapist from 8:30am to 9:00am. The ability to move my legs in weightlessness and at body temperature so I wasn’t feeling the cold was incredible. I wish we could have done this every morning.
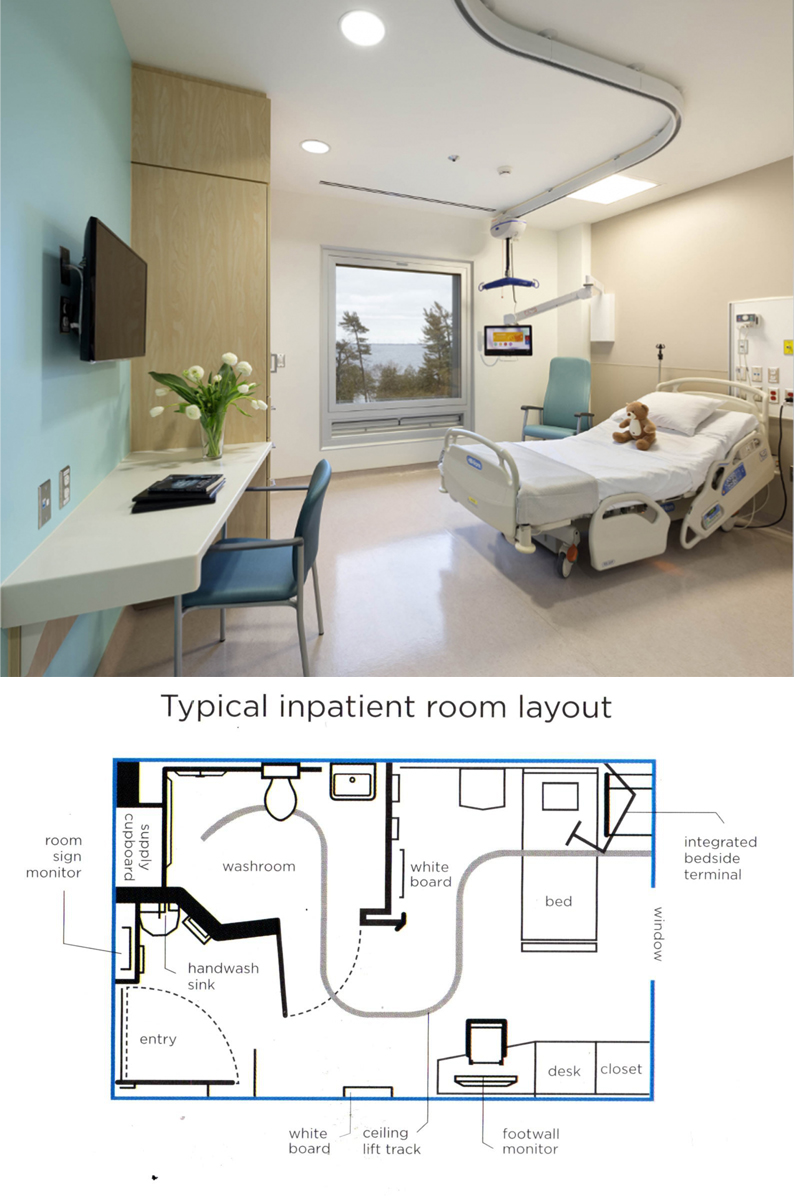 Having my own private room was a huge part of my convalescing process. It allowed me the privacy and space to reconnect with myself, instead of being in a hospital setting, a shared room, limited space, no ability or encouragement to get out and about in my wheelchair. I had a desk that I could set up my laptop on and work on my websites, social media and take care of business back on the farm and colour in my mandela colouring books.
Having my own private room was a huge part of my convalescing process. It allowed me the privacy and space to reconnect with myself, instead of being in a hospital setting, a shared room, limited space, no ability or encouragement to get out and about in my wheelchair. I had a desk that I could set up my laptop on and work on my websites, social media and take care of business back on the farm and colour in my mandela colouring books.
The food offered at PHC was exceptional and definitely a big part of the healing. Fresh salads with tomatos, cucumbers and other ingredients; homemade soups; homemade dinners with tasty sauces and fresh vegetables. Everyone of the patients that I talked with agreed and commented on the quality of the food that was provided. Good food contributes to physical strength, mental well-being, immunity and overall health.
Within the first day I was no longer using a bedpan. The PSW’s who were well trained in spinal cord injuries had me up and going onto the toilet without encouragement and not making me feel like I was imposing on them as I did when I was in the hospitals. Within less than 2 weeks I was independently transferring myself from my bed to my wheelchair, to the toilet and back to my wheelchair. Within a further week and a bit, I was able to shower independently own my own. The feeling of reaching this level of independence after spending three months on my back in hospitals was incredible.
Physiotherapy sessions moved forward on a steady pace. My therapists were definitely experts with spinal cord injury and they were amazing to work with. Always pleasant and the encouragement was phenomenal. The progress that I made over the seven weeks was incredibly inspiring. I learned a lot about myself, my capabilities and my limits. Dealing with my limitations and the setbacks due to the effects of chemotherapy on my body was disappointing to me and my therapists, but we persevered and the results still proved promising.
I was told by many of the physiotherapists and doctors in the hospitals that the damage to my spine was very severe and the prospects of walking were very slim. Here at PHC, I was encouraged to believe that the prospects of being able to walk to some degree in my life were absolutely possible. I was driven to prove this to be true.
At the time of my discharge, I was able to do what they called “non-functional walking” exercises whereby I would stand from my wheelchair and with the support of a two-wheel walker and a therapist on either side of me, I was able to walk 15 metres x 3 back and forth. I impressed myself and the therapists.
Unfortunately on the day before I was to be discharged I had a major setback that put me back at Kingston General Hospital for a week of tests. The upside to this setback is that I was discharged from KGH to home where with the help of my son and my daughter I have been able to carry on the exercises and therapy that I learned at PHC.
I repeat, the experience that I had at PHC remains and still is the greatest experience that I have had to date in staying in an institutional setting.