
June 2024
Are Poor Eating Habits Generational?
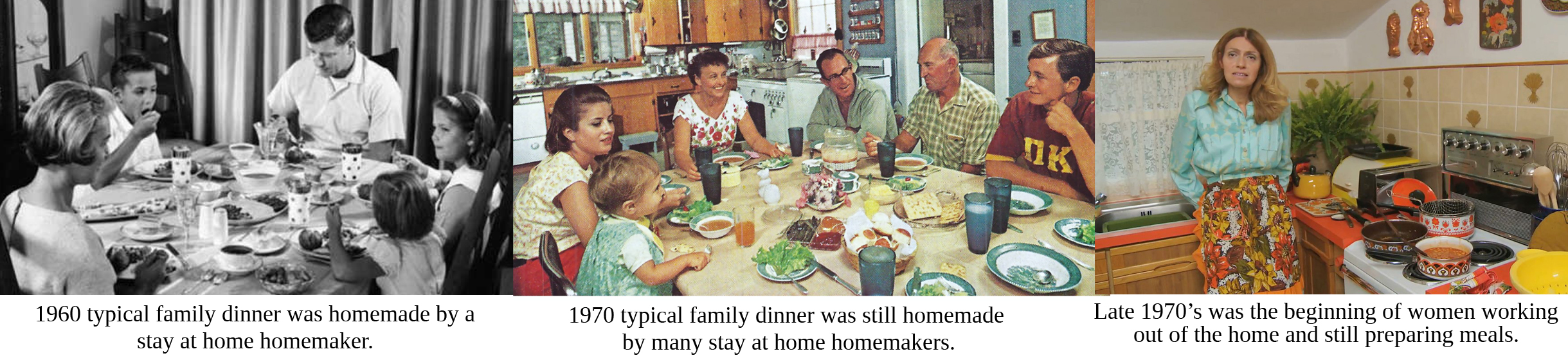
I must say, yes. Yes, I have been caught up in the generational wheel. I was raised in the 1960’s to 1980’s. Despite the fact that both my parents were raised on farms, their attitude towards farming was that it was a poor man’s lifestyle. They did not consider the quality of the food that they grew up with. My mother aspired to work outside the home. She did not want or desire to be a stay at home mother. She hated cooking and thus she cooked to live instead of living to cook. We grew up on quick meals, and junk food. My parents loved to entertain, so whenever they entertained the food flowed–steak, potatoes, vegetables, salads and alcohol. When I got married and started raising my own family, I inherited many of those traits, especially when it came to food. I did not live to cook, I cooked to live. I in turn fed my family grocery store discounted food, fast foods, and easy to cook meals.
In 2006, my son and I moved to our organic farm and started a lifestyle of being health conscious, paying attention to what we ate and where it came from. Unfortunately, for me, the damage to my health was done as a result of my childhood upbringing and the habits that I had developed over the years. Now I am faced with cancer. When I look at all the cancer diets and recommendations for nutritional and lifestyle changes, I don’t have to make many changes for my current condition. I just need to knuckle down more and get real serious about all aspects of my life. I invite you to join me on this journey to health and well-being starting here with food and nutrition.
Kathryn 
What is Para-Belly?
 When I woke up after my spinal cord injury, my belly was bloated. I asked what happened and I got no tangible answers. I had a very hard, washboard stomach with strong abs—this was not my body! What I was told was that I had para-belly which is common among spinal cord injury victims, especially when the thoracic spine has been affected. Apparently 'para-belly' is an abbreviation for paraplegic belly.
When I woke up after my spinal cord injury, my belly was bloated. I asked what happened and I got no tangible answers. I had a very hard, washboard stomach with strong abs—this was not my body! What I was told was that I had para-belly which is common among spinal cord injury victims, especially when the thoracic spine has been affected. Apparently 'para-belly' is an abbreviation for paraplegic belly.
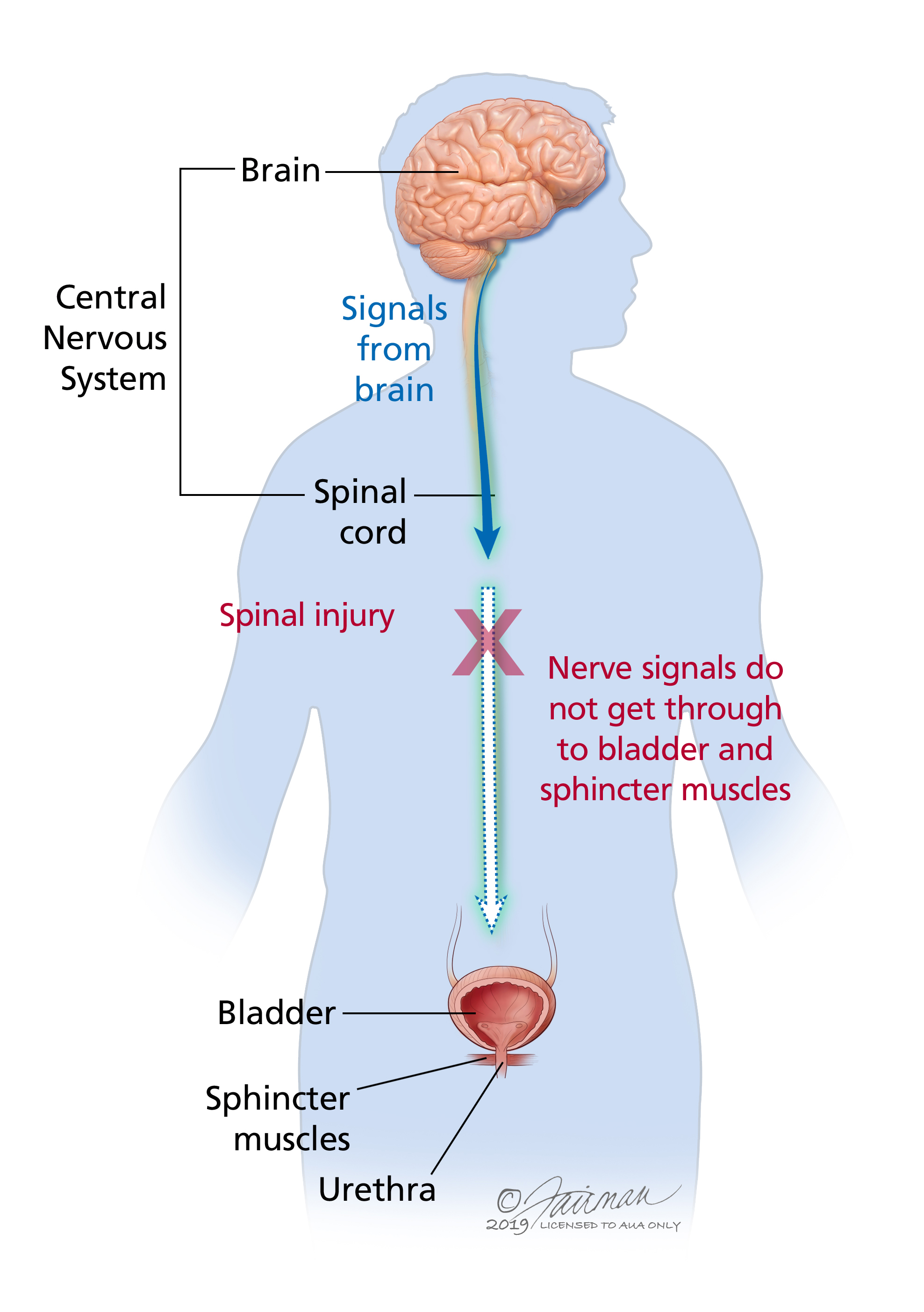
To this day, I have not found an answer to this question. From my own personal experience; whatever happened at the time of my SCI, the injury affected my bladder and my bowel functions and thus the belly bloat. I was able to finally talk to my new family doctor and all she could explain to me was that when there is an injury to the thoracic spine everything below the area of injury is affected and most times that affects the bowels and bladder. Many people not only have the belly bloat but have serious issues with toileting including having to do manual stimulation to both the bladder and the bowels on a regular basis as well as suppositories, enemas, and self-catheterization. It is a result of the brain being no longer able to talk to these organs. So how do they function? Something called sympathetic and para-sympathetic responses. This results in what is called neurogenic bladder or neurogenic bowels, which I discuss in more detail on my cancer page.
 I will continue to research this topic as I am still not happy with my research. If you have anything you wish to comment on or share, please do.
I will continue to research this topic as I am still not happy with my research. If you have anything you wish to comment on or share, please do.
I do know from watching videos and doing my own research that a washboard abdomen can be achieved after a spinal cord injury with a lot of exercise, patience and time. See my page on exercise for exercises to help strengthen abdominal muscles.
With ongoing research, I was able to find the following article which indicates that what I am referring to as para-belly or belly bloat after a spinal cord injury is referred to as 'upper gastrointestinal dysmotility' which is described in detail.
CLICK HERE for the full article.
The following article discusses the subject of gastrointestinal dysfunction after a spinal cord injury which leads to para-belly or belly bloat and a number of other gastrointestinal issues, which unfortunately are a life-long disfunction of the body due to the SCI.
CLICK HERE for the full article.
Kathryn 
Testimonial to Providence Spinal Cord Rehabilitation
I spent seven weeks at Providence Health Care facility in Kingston, Ontario from March 21 to May 12, 2024. It was and still remains the best experience of my 7 out of 9 months in hospital institutions this past year.

Upon being admitted to PHC, I was greeted by a barrage of friendly faces of nurses, PSW’s, PSA’s, students and doctors. I was assigned two physiotherapists, one for my actual physiotherapy and the other which would also provide physiotherapy but their focus would be more getting me back home into an environment that would work for me. They would assist me with various ways to transfer to and from my wheelchair, getting me properly fitted for the ideal wheelchair and helping me to order that ideal wheelchair. We practiced transfers to and from a mock up vehicle that could be programmed to the height of my vehicles. We practiced transfers to and from the toilet, the bed and we went outdoors and practiced going across grass, up and down ramps and across gravel with my wheelchair.
My day started out by waking up around 6:30am, getting dressed and then doing stretching exercises in my bed. Breakfast was served between 7:30am and 8:00am. I would then go down the hall and do an upper body workout on the arm machine and then do a couple laps down the hall to the cafeteria and back in my wheelchair. Morning therapy session was from 10am to 11am. Lunch was as 12 noon in the common room. Another physiotherapy session in the afternoon from 2pm to 3pm followed by dinner at 6pm back in my room. More laps up and down the halls and free time to read, meditate or nap in my room. Lights out or bedtime was on our own. Evenings could be spent socializing with the group that would come together by the nurses station, do laundry and watch TV in the common room or in my own private room.
One of the therapies that I looked forward to was time in the heated, salt water therapy pool. Two to three times a week with my therapist from 8:30am to 9:00am. The ability to move my legs in weightlessness and at body temperature so I wasn’t feeling the cold was incredible. I wish we could have done this every morning.
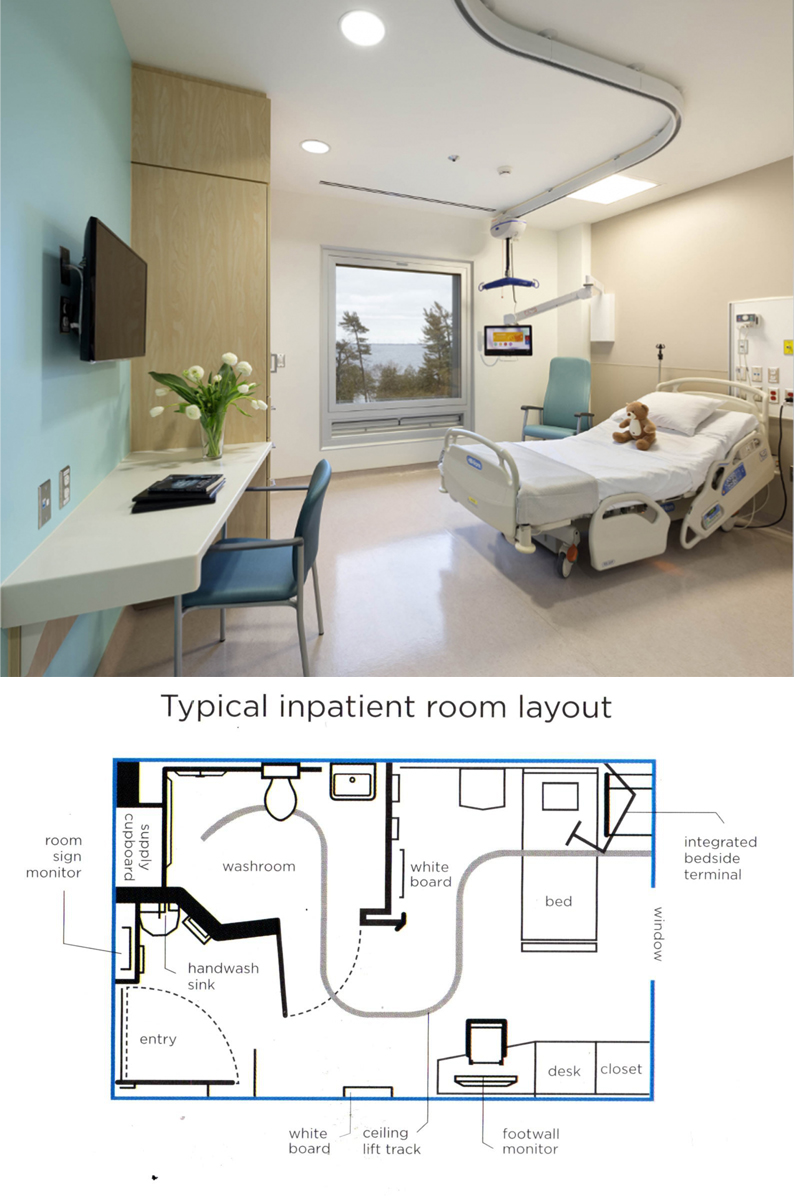 Having my own private room was a huge part of my convalescing process. It allowed me the privacy and space to reconnect with myself, instead of being in a hospital setting, a shared room, limited space, no ability or encouragement to get out and about in my wheelchair. I had a desk that I could set up my laptop on and work on my websites, social media and take care of business back on the farm and colour in my mandela colouring books.
Having my own private room was a huge part of my convalescing process. It allowed me the privacy and space to reconnect with myself, instead of being in a hospital setting, a shared room, limited space, no ability or encouragement to get out and about in my wheelchair. I had a desk that I could set up my laptop on and work on my websites, social media and take care of business back on the farm and colour in my mandela colouring books.
The food offered at PHC was exceptional and definitely a big part of the healing. Fresh salads with tomatos, cucumbers and other ingredients; homemade soups; homemade dinners with tasty sauces and fresh vegetables. Everyone of the patients that I talked with agreed and commented on the quality of the food that was provided. Good food contributes to physical strength, mental well-being, immunity and overall health.
Within the first day I was no longer using a bedpan. The PSW’s who were well trained in spinal cord injuries had me up and going onto the toilet without encouragement and not making me feel like I was imposing on them as I did when I was in the hospitals. Within less than 2 weeks I was independently transferring myself from my bed to my wheelchair, to the toilet and back to my wheelchair. Within a further week and a bit, I was able to shower independently own my own. The feeling of reaching this level of independence after spending three months on my back in hospitals was incredible.
Physiotherapy sessions moved forward on a steady pace. My therapists were definitely experts with spinal cord injury and they were amazing to work with. Always pleasant and the encouragement was phenomenal. The progress that I made over the seven weeks was incredibly inspiring. I learned a lot about myself, my capabilities and my limits. Dealing with my limitations and the setbacks due to the effects of chemotherapy on my body was disappointing to me and my therapists, but we persevered and the results still proved promising.
I was told by many of the physiotherapists and doctors in the hospitals that the damage to my spine was very severe and the prospects of walking were very slim. Here at PHC, I was encouraged to believe that the prospects of being able to walk to some degree in my life were absolutely possible. I was driven to prove this to be true.
At the time of my discharge, I was able to do what they called “non-functional walking” exercises whereby I would stand from my wheelchair and with the support of a two-wheel walker and a therapist on either side of me, I was able to walk 15 metres x 3 back and forth. I impressed myself and the therapists.
Unfortunately on the day before I was to be discharged I had a major setback that put me back at Kingston General Hospital for a week of tests. The upside to this setback is that I was discharged from KGH to home where with the help of my son and my daughter I have been able to carry on the exercises and therapy that I learned at PHC.
I repeat, the experience that I had at PHC remains and still is the greatest experience that I have had to date in staying in an institutional setting.